
Discovery Hints at Genetic Basis for the Most Challenging Symptoms of Schizophrenia
Study suggests that current medications don’t target the right neural pathways to treat cognitive deficits often associated with the disease
Our understanding of schizophrenia has increased greatly in recent years, as studies of large groups of people have identified a multitude of genetic variants that increase a person’s risk of the disease. But each of those individual risk factors accounts for “only a very minor amount of the overall risk,” said Alex Nord, a professor of neurobiology, physiology and behavior in the College of Biological Sciences and the Center for Neuroscience.
Now a team of researchers co-led by Nord and graduate student Tracy Warren has connected genetic variants to the neural pathways that underlie some of the most challenging aspects of schizophrenia.
“This is a new approach,” said Nord. “To have this level of detail is really powerful.” The results were published March 15 in Molecular Psychiatry.
The work could one day lead to better diagnosis and treatment for the most devastating symptoms of schizophrenia – the ones most likely to leave a person homeless or unemployed – but least likely to respond to current medications.
A constellation of symptoms
Schizophrenia is often seen as a disorder of delusions and hallucinations, but the reality is more complex. People with the disease often suffer an array of symptoms, such as loss of motivation, inability to experience pleasure, social withdrawal, emotional flatness and even a tendency not to speak. Months or years can pass before a person is properly diagnosed and treatment is started — during which they can experience frayed relationships, lost jobs and deteriorating school performance. People with schizophrenia can also experience impaired cognitive control, making it difficult to organize their thoughts or direct their attention.
“These symptoms are some of the strongest predictors of negative life outcomes” such as unemployment, divorce, or homelessness, said Warren. Although existing medications can often curb hallucinations and delusions, “currently, we don’t have the drugs to fix these other symptoms.”
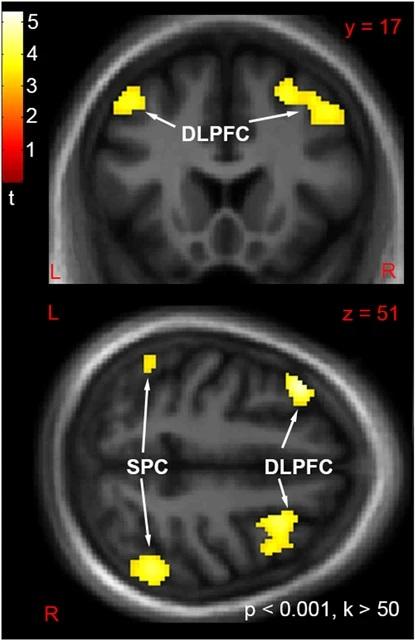
Warren and Nord set out to study how genetic variants that are risk factors for schizophrenia actually contribute to the disease. They collaborated with Dr. Cameron Carter’s team at the Early Diagnosis and Preventive Treatment (EDAPT) Clinic, which offers psychosis care through the UC Davis School of Medicine and the Department of Psychiatry and Behavioral Sciences. Working with Carter and his team at EDAPT, Warren analyzed DNA from 205 patients and 115 healthy people. Carter’s team had examined these subjects in great detail, including interviews, cognitive tests, monitoring changes in their disease over time, and functional brain imaging to show how different brain areas worked together during mental tasks.
This rich patient and genetic dataset allowed Warren to attempt something new: examining genes linked to specific neural pathways to see if they are drivers of particular schizophrenia symptoms. Dr. Pak Sham at the University of Hong Kong was brought in as an expert on the genetic epidemiology of psychiatric disorders.
Working with Justin Tubbs, who was then a graduate student in Sham’s lab, Warren profiled these subjects against variants in more than 1,000 genes affecting four different neurotransmitter pathways — dopamine, GABA, glutamate, and serotonin.
Warren and Tubbs found that genetic variants in the glutamate and GABA pathways were strongly associated with deficits in cognitive control and social problems — a result that “was really interesting,” said Warren, because it hints at new strategies for treating the disease.
Treating the right neural pathway
Medications that are currently available for schizophrenia generally target dopamine and are usually effective in reducing hallucinations and delusions. But the new results suggest that cognitive problems — which greatly impact a person’s life trajectory — are driven by neurotransmitter pathways that aren’t targeted by current medications.
“This validates that we need to keep looking for treatments targeting these other pathways,” Warren said.
When Warren divided the patients into clusters according to their individual groupings of disease symptoms and genetic variants, she found that patients with serious symptoms naturally separated into two subgroups — those who primarily experience cognitive problems, and those who primarily have hallucinations and delusions. Those with hallucinations and delusions usually respond well to existing medications, but those with cognitive problems do not.
Studies like this one could eventually pave the way toward more effective care for people with schizophrenia, Warren said. “I would love to see people genotyped in the psychiatry clinic, have their neurotransmitter pathways examined, and their treatments selected based on this.”
Nord believes that this approach, with early genetic testing, could also streamline the process of diagnosing schizophrenia and starting treatment. Diagnosis often consumes many months, allowing symptoms to worsen, yet the longer treatment is delayed, the more difficult it is to treat the disease.
“Twenty years from now, we could potentially connect people with treatment earlier, before the symptoms become devastating,” he said.

A leap of faith
For all this success, Nord admits that he was initially reluctant when Warren wanted to attempt this study — to use genetic data to connect neural pathways with symptoms. In a world where identifying the genetic risk variants required over 100,000 patients, it seemed far-fetched to think that they could take this next step with only 320 subjects.
“I honestly didn’t know if it would work,” said Nord, who has spent two decades in research. “Tracy really did drive this. It was a situation where the graduate student teaches us something.”
Additional authors on the paper are: at UC Davis, Tyler A. Lesh, Mylena B. Corona, Sarvenaz S. Pakzad, Marina D. Albuquerque, and Praveena Singh; at UC Davis and Northwestern University, Vanessa Zarubin; at UC Davis and Washington University in St. Louis, Sarah J. Morse.
Media Resources
- Douglas Fox is a freelance science writer based in the Bay Area.
- Nord Lab
- Sham Lab
- Carter Lab
- Association of neurotransmitter pathway polygenic risk with
- specific symptom profiles in psychosis (Molecular Psychiatry 2024)